Prostate Cancer: Radiation Therapy.

Well my last topic for therapy in regards to prostate cancer was on surgery. Today I will be tackling the topic of Radiation Therapy and how it relates to prostate cancer. Since this month is Prostate Cancer Awareness, I think it is best to try and describe the different treatment options that are available to our patients. Remember, the size of the prostate is only about the same size as a walnut.

To get started, let me give you a brief over view:
Radiation therapy, or radiotherapy, is a common way to treat prostate cancer. Doctors who specialize in treating cancers with radiation are known as radiation oncologists. In radiation therapy, high-energy x-rays are used to kill cancer cells. In early stage prostate cancer, radiation can be used instead of surgery, or it may be used after surgery to destroy any cancer cells that may remain in the area. In advanced stages of prostate cancer, it may be given to relieve pain or other problems.
Radiation therapy can be given in a variety of ways. The two most common ways that radiation therapy are delivered are through external beam radiation therapy and brachytherapy. External beam radiation therapy (EBRT) involves the delivery of radiation via a machine that aims x-rays at the body. During brachytherapy or interstital implantation, a physician places small pellets or seeds of radioactive material directly into the prostate gland Most patients receive one or the other kind of radiation and some patients receive both kinds of radiation therapy.
External Beam Radiation Therapy:
External beam radiation therapy (EBRT) for prostate cancer is given on an outpatient basis, 5 days a week, for approximately 6 to 8 weeks. EBRT begins with a planning session, or simulation, where marks are placed on the body and measurements are taken in order to line up the radiation beam in the correct position for each treatment.
This is what the marks look like on a patient:
 You can see that there is a tiny little dot in the middle of the patient. We then shine light lasers onto the skin and use these to align our patients underneath the machine and in simulation.
You can see that there is a tiny little dot in the middle of the patient. We then shine light lasers onto the skin and use these to align our patients underneath the machine and in simulation.
Patients lie on a table and are treated with radiation from multiple directions to the pelvis. The actual area of the pelvis receiving radiation treatment may be large or small, depending on the features of the cancer.
Here is another example of what it is like for a patient:
 As you can see, the lights are shining on the patients skin. This allows the therapists to ensure that the patient is laying under the machine exactly where they are supposed to be placed for their treatment. Once the patient is aligned, and everything on the monitor says that the patient is in the correct position, we can then treat the patient with radiation to the prostate.
As you can see, the lights are shining on the patients skin. This allows the therapists to ensure that the patient is laying under the machine exactly where they are supposed to be placed for their treatment. Once the patient is aligned, and everything on the monitor says that the patient is in the correct position, we can then treat the patient with radiation to the prostate.
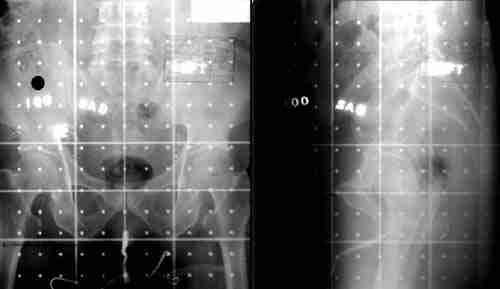
Radiation can be delivered specifically to the prostate gland (prostate only radiation) or encompass the surrounding pelvic lymph nodes in addition to the prostate gland (whole pelvic radiation). Patients who are receiving treatment to a larger area of the pelvis may undergo another planning session to focus the radiation to the prostate gland, where cancer cells are greatest. Here is an Xray of what that would look like:
As you can see in the above photograph or Xray. This is the patients pelvis, and by the boney anatomy, we can tell that we have the entire prostate and most of the nodes of the prostate in this field area for treatment. If you look closely, you can see a small little round shadow in the left picture, this would be representative of where the prostate is located.
Some radiation therapy centers will use a special CT scan and computer prior to the planning session to better locate the prostate gland and more precisely aim the radiation. This capability is known as three-dimensional conformal radiation therapy, or 3D-CRT. The use of 3D-CRT appears to reduce the chance of injury to nearby body structures, such as the bladder or rectum. Since 3D-CRT can better target the area of cancer, radiation oncologists are evaluating whether higher doses of radiation can be given safely while achieving greater cure rates. Preliminary data from several cancer programs suggests that the higher radiation dose delivered with 3D-CRT can reduce the rate of local cancer recurrence.
This is what a typical 3D Treatment plan for the prostate might look like:

There is yet another form of EBRT, or external beam radiation therapy that is even a step better then the 3D Radiation Therapy, this form is called IMRT. IMRT is an acronym for Intensity Modulated Radiation Therapy. A simplistic definition of IMRT is that it allows physicians and dosimetrists (the ones that plan radiation treatments on a computer) to "paint" high doses of radiation to the prostate itself, and limit or decrease the amount of radiation delivered to normal tissues. This again allows physicians to delviery very high doses of raidation to the prostate cancer, and lower doses to normal tissues. This helps to achieve better survival rates and cures for patients, with lower chances for side effects from the treatments as well. To give you an idea of how precise IMRT can be, one can change the amount of radiation from 100% to less then 50% in less then a 3mm space. That is incredible! Here is a couple pictures of what an IMRT plan would look like:
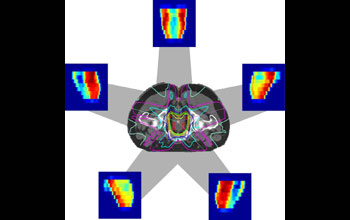
This above picture demonstrates the differences in the doses being administered. The RED color is the higer areas of radiation and the blue and green colors are the colder or less areas of radiation. You can also see how there is less radiation going to smaller areas of normal tissues in the body as well.

This picture shows another IMRT treatment that was planned for a patient as well. You can see the different areas in which the beams enter the body, and then they all converge and concentrate on the prostate itself, where you see the red spots, and the highest areas of radiation. You get very low areas of radiation exposure outside of the prostate since IMRT is being used.
Interstitial Brachytherapy:
Internal radiation is known by a number of names: "interstitial brachytherapy," "seeds," or "implantation." These terms refer to treatment where radioactive material is placed directly into the prostate gland. For prostate cancer, the most common method of interstitial brachytherapy is permanent implantation of radioactive seeds into the prostate gland through the perineum. This is an example of what the seeds look like, and the size of them as well:

The perineum is the area of skin between the scrotum and the anus. The implantation procedure is performed in the operating room while the patient is asleep or numb from the waist down. An imaging device known as an ultrasound is inserted into the rectum to visualize and guide placement of the seeds with needles into the prostate. Here is an example from an OR case:

After the procedure, the patient will temporarily contain a small amount of radiation from the seeds, although this amount is not generally dangerous to most other people. Some doctors may advise patients to avoid close contact with young children or pregnant women for several weeks.
This is what the actual plan of a prostate implant, or brachytherapy procedure looks like:
 (This is a 3D rendering of what the plans inside the patient looks like.)
(This is a 3D rendering of what the plans inside the patient looks like.)

This is what the plans looks like to the physician as he is doing the procedure in the OR with the Uroligist and the patient.
This final Xray is what the pelvis then looks like under an Xray film with all of the seeds placed into the patient and into the prostate.

As you can see there are lots of seeds that are inserted into the prostate in order to best allow for enough radiation to be delivered to the patient and the prostate cancer. In most cases there are typically 80 to 120 seeds inserted into the prostate. It all varies from patient to patient, and based on diagnoses of the disease.
I hope this helps answer some questions and gives some information about Radiation Therapy when it comes to treating prostate cancer. If you have any other questions or concerns, or want to ask me about anything else, please contact me at: CANCERGEEK@GMAIL.COM
~CancerGeek