19 Oct Breast Cancer: IMRT
Today I want to take some time and touch on a topic that is up for some debate. The use of IMRT (Intensity Modulated Radiation Therapy) in the use of breast cancer. First off, it is probably important to explain exactly what IMRT is and what it does.
IMRT is like painting with radiation. As you can see in this picture of Einstein, which was made by a linear accelerator, using IMRT to do so. It allows the physician and dosimetrist to create a plan that allows us to deliver a high amount of radiation to the areas that are very important to get a radiation dose to, such as the lumpectomy cavity, and then to decrease and limit the amount of radiation exposure to normal and critical organs, such as the lung or the heart on a left sided breast cancer. In the example above, the darker areas would be those exposed to more radiation, and the lighter areas received less amounts of radiation. You can see how precise this can be when done correctly.
Know that we know what IMRT is, and a simplistic definition of what its purpose is set to accomplish, I think it is now appropriate to take a closer look at IMRT for Breast Cancer. The traditional or standard or care for breast radiation is a 3D plan typically consisting of two tangential fields. It may look something like this:
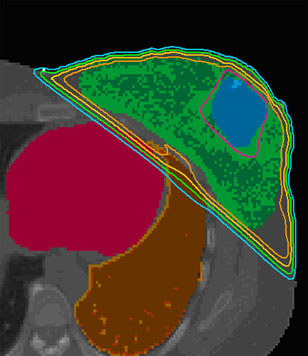
As you can see in the above picture, there would be a field that comes from the upper left hand side, and entering the patient, and another field that would be coming from the bottom right hand side and then entering the patient as well. Since this is a left sided breast cancer, you can also that there is a small portion of lung (orange color) and heart (pink/magenta color) that is included in the treatment fields.
Since the breast tissue goes all the way down to a patients chest wall, or for simplicities sake, rib cage, there has traditionally been about 1.5 to 2.0cm of lung included in most physicians breast plans. This is to ensure that all of the breast tissue is being included in the radiation field, and that even with the motion of patient breathing, that the breast is always targeted with the radiation that is being administered to the patient.
In this slide above, you can see the difference between a breast IMRT plan (Left) and a conventional “standard of care” plan on the right. If you pay close attention to the images on the right hand side, you will notice the arrows pointing towards the areas labeled hot spots. This is the one down fall with conventional, or tradition breast radiation. The radiation is trying to be delivered to a large area of tissue, and trying to deliver and dose that is the same through out. Unfortunately, we all know that breast tissue is not a nice little box that is the same size in all directions.
Due to this factor alone, there tends to be these hot spots in the areas of breast tissue that happen to be thicker, have more tissue overlapping itself, such as underneath the breast tissue and next to the rib cage of a woman, or perhaps where there is not enough breast tissue. We then try to “compensate” for this difference in breast tissue with the use of a device that we call a “wedge”.

In these instances, patients may end up having some skin reddening or even experience the skin breaking down and in some situations, a severe burn and weeping of the skin happens.

The above photo happens to be a more severe case of what a patient may experience. As I said, not all patients experience a case to this extreme, but I think the point and case is made that there is an increase in radiation delivered to some of these areas of the breast that do not need that much radiation, and with that, comes some unnecessary skin reactions that a woman should not have to go through if at all possible.
This is where IMRT comes into play.
IMRT is made up of many tiny little beams about the size of a pencil referred to as beam-lets. These beam-lets can be thought of like an older dot matrix printer. In using all of these small little numerous beam-lets, to form one larger beam, it allows the physician and the dosimetrist to develop a highly conformal and precise delivery of radiation to the patients.

Again in this picture you can see the difference between the two plans. The one of your left is the typical conventional plan and the one on your right is the IMRT plan. You can see first hand how the IMRT plan on the right allows the radiation oncology team to focus the field more intensely on the tumor area itself and limit the dose to nearly normal tissues.
In order to accomplish this, the physician needs to plan ahead and really think through his outcome that he ideally would like for the patient. The physician will have to look at all the scans, and then actually sit down at a computer and contour, or draw over all of the breast tissue that he wants to be treated. He will then also need to draw other areas of interest that he may want to avoid, such as the lung or the heart if a left sided breast cancer. At times physicians will also make sure to draw a seperate area around the lumpectomy cavity, where the tumor was removed. This is to make sure that this area received a bit more radiation then the rest of the breast tissue. The rationale is that close to 85% of the time if a patient is going to recur, its going to be locally at the sight where the original tumor was located.
Once this is all done, the computer is then put to work to develop a plan that will achieve all of the physicians desired outcomes and taking into consideration the limitations that the physician also wants to consider. For example, the physician wants the entire Breast to be treated to a dose of 50.4cGy, and wants the lumpectomy area to get a bit more radiation, and go to a dose of 60.4cGy. Perhaps the physician wants to limit the amount of radiation to the heart to less then 10% of the total dose, and wants there to be no hot spots greater then 5mm in any dimension. The computer takes all of this into consideration, and the dosimetrist helps to maneuver the plan in order to get the outcomes that the physician wants for his patient.
What happens is that a plan is generated that allows little deposits of varying doses to be places all along the breast tissue in order to achieve the type of outcome and plan that the physician would ideally like for his patient. It may look something like this:

In this view, you can see the different columns are at different heights. This represents the amounts of radiation being deposited in any one particular area of the breast tissue. The largest columns may be right at the original sight of where the tumor was located. The area that is the shortest in height may be at the underside of the breast, where a skin reaction is most likely to occur. In doing this, it allows the radiation to be “painted” onto different areas within the breast tissue at different intensities.
So why is all of this important and why do we need Breast IMRT?
1. More conformal dose to the Breast: The natural taper of the breast produces hot spots in ranges of 3% to 20%. Even with the use of wedges, these hot spots are still very noticeable and can still produce some substantial side effects for patients. IMRT can drastically reduce these hot spots.
2. Lower dose to the Heart and Lungs: Dose is fairly low in all cases on left sided breast cancers, however, with the use of IMRT the dose that is administered to the heart and lung can be lowered even more. In one study done abroad, it was shown that the dose to the left lung and ventricle could be reduced to less than 500cGy, or less then 10% of the prescription dose. In patients that have pre-existing conditions such as Congestive Heart Failure or decreased lung function, this improvement can be drastically significant in their overall health.
3. Lower dose to the opposite breast: In some recent data published be a group from the Netherlands and presented at ASCO, they took a look at 999 women that were previously treated for Breast Cancer. What they saw was that in women ages 40 years and younger, that they had an increase risk of developing Breast Cancer in their opposite breast by as much as 60%. IMRT can drastically reduce the amount of radiation being deposited to the opposite, or unaffected breast in comparison to the scatter radiation it typically receives from conventional methods.
4. Field with in a field: The fact that IMRT allows physicians to increase the amount of radiation being deposited in a certain area means that a patient can receive their overall breast radiation as well as their boost to the tumor site at the same time. This decreases the overall number of times that a patient has to come in for their radiation treatments. This can be a bit more convenient for patients.
As always, if you or a loved one have any other questions, comments, or concerns; if you would like more information in regards to another cancer related topic, please contact me at: CANCERGEEK@GMAIL.COM or CANCERGEEK@CANCERGEEK.COM
~CancerGeek


Pingback:www.topcholesteroladvice.info » Breast Cancer: IMRT
Posted at 03:48h, 20 October[…] cancergeek added an interesting post today on Breast Cancer: IMRTHere’s a small readingIn patients that have pre-existing conditions such as Congestive Heart Failure or decreased lung function, this improvement can be drastically significant in their overall health. 3. Lower doese to the opposite breast: In some recent … […]
Pam
Posted at 07:06h, 25 OctoberThank you for such an informative article on IMRT. I am undergoing IMRT treatment for left sided breast cancer. I have just been informed by my secondary health insurance (Tricare 4 Life) that they will not cover the payment for this treatment. They consider it experimental. Everything I have read and everything my doctor has told me has convinced me that this is the best treatment for me. I have an enlarged atrium of the heart which the cardiologist said was probably due to my hypertension. I also have a 25+ year history of SVT. With this history do you think choosing IMRT over conventional radiation treatment for breast cancer was the best decision?
loan for debt consolidation loan
Posted at 13:56h, 10 Januaryerr I keep getting an error when trying to skip to the next article
Kitchener mortgage
Posted at 08:56h, 21 FebruaryJust a quick comment 2 thx u for your interesting page article. Do u know where I can find more on this? well done. Tracy x
Beatrice
Posted at 04:07h, 15 MarchThis is the perfect way to break down this innmoratiof.