04 Oct Breast Cancer: Mammosite
 Since it is Breast Cancer Awareness month I think it would be a great time to discuss some of the new research and technological advnaces that have been in made in the treatment options for women with early stage Breast Cancer. No longer are the only choices for women with early stage Breast Cancer confined to mastectomy (loss of all breast tissue) or Whole Breast Irradiation (Radiation Therapy).
Since it is Breast Cancer Awareness month I think it would be a great time to discuss some of the new research and technological advnaces that have been in made in the treatment options for women with early stage Breast Cancer. No longer are the only choices for women with early stage Breast Cancer confined to mastectomy (loss of all breast tissue) or Whole Breast Irradiation (Radiation Therapy).
Some of these new advances include Lumpectomy (removal of the the tumor), Sentinel Node Biopsy (to see if tumor has spread), Chemoprevention (use of drugs to prevent breast cancer), and Partial Breast Irradiation, or commercially sold as Mammosite. Today I want to focus strictly on Mammosite and Partial Breast Irradiation.
Before I get into Mammosite and what it is, I think it is important to have a visual image of the size of an early stage breast cancer. This way patients have an idea of how large or small a breast cancer can be when first diagnosed:

Mammosite is a treatment option for a select group of women with early stage breast cancer. This treatment option will include a lumpetcomy, or the surgical removal of the cancer itself from the breast. After the lumpectomy has been performed, women should then be referred to a Radiation Oncologist for a consult. According to the NCCN guidelines, 100% of women that have receive a lumpectomy should be referred on for radiation.
Historically, women then received radiation to the entire breast 5 days a week, for an average of 6.5 weeks. Women would experience fatigue, skin irritation, and at times a bad burn on the skin that could even break open from time to time. This is an example of a tradiational 3D Conformal Whole Breast Radiation Plan:
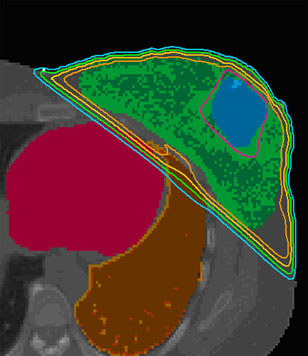 As you can see in this diagram, the entire breast is being encompassed by the colored lines. The colored lines refer to the percent of radiation at different depths that the breast tissue is receiving. The cyan, or aqua color refers to the 95% line.
As you can see in this diagram, the entire breast is being encompassed by the colored lines. The colored lines refer to the percent of radiation at different depths that the breast tissue is receiving. The cyan, or aqua color refers to the 95% line.
In this next photograph, you will see an example of how badly the skin can get burned with whole breast radiation.
 As you can see, the skin directly under the breast, next to the chest and upper abdomin area have gotten severely red and burned. Due to the radiation entering the body from the outside, and then entering into the body to treat the breast cancer, the skin is affected as well. This is because the entire breast was in the field, and as the breast tissue overlaps and sits on top of the abdomen, a build up effect occurs and causes this skin burn reaction.
As you can see, the skin directly under the breast, next to the chest and upper abdomin area have gotten severely red and burned. Due to the radiation entering the body from the outside, and then entering into the body to treat the breast cancer, the skin is affected as well. This is because the entire breast was in the field, and as the breast tissue overlaps and sits on top of the abdomen, a build up effect occurs and causes this skin burn reaction.
Then in 2002 a new device received FDA clearance, that device was called Mammosite. Mammosite is a device that also administers radiation to the breast. Instead of the entire breast being exposed to radiation from the outside in, it treats the breast cancer area from the inside out. The thought process was that if we can treat the breast cancer from within, we can then alleviate some of the side effects that women have experienced with traditional radiation therapy. Mammosite decided to take it one step further, and say that if you remove the cancerous lesion with a lumpectomy, then why not just irradiate the cavity where you removed the breast cancer and a small area surrounding it, and NOT the entire Breast.
In 2002, after a 5 year study performed by Mammosite with their technology, the FDA cleared Mammosite to be used clinically for early stage Breast Cancers. The study that was performed by Mammosite consisted of 43 patients. The 43 patients were followed up for a total of 5 years. These patients had early stage Breast Cancer consisting of either DCIS or invasive ductal carcinoma. The patients had a lumpectomy to surgically remove the lesion from the breast. Then a catheter with a small balloon was placed in the cavity.
This is what the balloon looks like:

This allows Mammosite to be applied to the tumor bed (area where tumor used to be:lumpectomy site). Patiend would then receive a total of 10 treatments spread over 5 days in a row. Patients would receive a treatment in the morning, wait at least 6 hours in between, and then receive a second treatment later that day.
This is a picture of a radiation plan of a Mammosite patient:

Of the 43 patients in the trial, 0 (none) patients had a local recurrence. An astounding 97% of patients had a good/exceleent cosmetic result according to the American Brachytherapy Society. Mammosite will actually report a slightly lower percentage and say that it was 82% of patients had a good/excellent cosmetic result. Of all 43 participants asked if they would do it over again or recommend this treatment to a family member, 100% of the patients said YES they would.
How Mammosite works?
1. Placement

After the breast cancer tumor is removed (lumpectomy), a small, soft MammoSite balloon attached to a thin tube (catheter) is placed inside the lumpectomy cavity through a small incision in the breast.
- The balloon is “inflated” with saline solution so that it fits snugly into the cavity. It remains inflated during the 5-day treatment.
- A small portion of the catheter remains outside the breast; this is secured to a cushioned gauze pad to prevent movement of the catheter.
2. Treatment

- Treatment is planned by a radiation oncologist who will take images of the MammoSite balloon catheter in the breast and determine the amount of radiation needed.
- During therapy, the portion of the catheter that remains outside your breast is connected to a computer-controlled High Dose Rate (HDR) machine that inserts a radiation “seed” to deliver the therapy.
- Once therapy is complete, the seed is removed, the catheter is unplugged, and you will be free to return to your normal daily activities.
- No radiation remains inside your breast in between treatments.
3. Removal

- After 5 days of treatment, your MammoSite balloon catheter will be removed, usually on the last day of treatment.
- The balloon is gently removed through the same incision made to place it.
What are some of the advantages of Mammosite?
- Treatment course is only one week as compared to 6.5 weeks of radiation therapy.
- The treatment is applied directly to the area in which the breast cancer was removed. This is also the spot where the breast cancer is the most likely to recur.
- Clinical trials have shown Mammosite to be well tolerated by patients even with an increased Radiation dose over a shorter amount of time for the treatment.
- More convienent for patients that might be further away from a cancer center, since the course of treatment is only 5 days versus 6.5 weeks.
Is Mammosite right for me?
Accoriding to two seperate Medical Societies, the American Society of Breast Surgeons and the American Brachytherapy Society, here are there patient selection criteria for women with early stage breast cancer:
| Society Recommendations | ||
| American Society of Breast Surgeons12 www.breastsurgeons.org |
American Brachytherapy Society13 www.americanbrachytherapy.org |
|
| Age | ≥45 | ≥50 |
| Diagnosis | Invasive ductal carcinoma or DCIS | Unifocal, invasive ductal carcinoma |
| Tumor Size | ≤3cm | ≤3cm |
| Surgical Margins | Negative microscopic surgical margins of excision | Negative microscopic surgical margins of excision |
| Nodal Status | NØ | NØ |
With the advancement of technology and the clinical trials from the Mammosite, it has led researchers to want to gain more information. There is currently a phase III trial under way sponsered by the National Cancer Institute (NCI) and being ran by the National Surgical Adjuvant Breast and Bowel Project (NSABP) in conjunction with the Radiation Therapy Oncology Group (RTOG) looking mroe specifically at the difference between parital breast irradiation (Mammosite and other like techniques) versus conventional whole breast irradiation for women with Stage 0, 1, or 2 Breast Cancer. I will discuss this Phase III trial more in depth tomorrow.
As always, if you or a loved one have any other questions, comments, or concerns; if you would like more information in regards to another cancer related topic, please contact me at: CANCERGEEK@GMAIL.COM or CANCERGEEK@CANCERGEEK.COM
~CancerGeek

Pingback:Day 0 – Chemotherapy 1 My Breast cancer (Vitamin B17 deficiency) recuperation journey – To Live 100 Years
Posted at 14:53h, 20 January[…] foci suspicious for perineural invasion, tumor within 0.1cm of the nearest surgical margin. (See cancergeek blog for the Early Stage cancer […]