05 Oct Breast Cancer: Phase III Trial
As I mentioned in yesterday’s blog on Mammosite, today I was going to talk a little more in depth about the phase III randomized trial that is underway. This NSABP-RTOG Phase III trial is entitled: Conventional Whole Breast Irradiation versus Partial Breast Irradiation for Women with Stage 0, 1, or 2 Breast Cancer. The protocol number respectively are: NSABP-B39 and RTOG-0413.
The purpose of this trial is to evaluate the difference, if any, between women that recevie radiation to the entire breast as comopared to women that receive radiation to just the lumpetcomy cavity only. The investigators want to know if only treating the site where the tumor was located is as effective as treating the entire breast to provide women with local tumor control, disease free survival, and distant disease free survival. The investigators also are taking into consideration the patients’ quality of life, cosmetic outcome, fatigue, treatment related symptoms, and the patients’ perception on the conveneince of care.
In order for patients to qualify for this study the hospital or institution that they are going to for treatment must be affiliated with either RTOG, NSABP, or the NCI. Patients must also either be Stage 0 (DCIS), 1, or 2 and ahve no evidence of any metastatic disease. In other words, your breast cancer had to be confined to the breast area only, and it had to be a smaller sized tumor. The maximum size for tumor/lumpectomy site was 3 cm. Women would undergo a lumpectomy, and the pathology had to come back that the margins were negative for any further disease. If patients had positive axilliary nodes, it had to be restricted to 3 nodes or less in order to qualify for the study. Patients will be stratisfied based on disease stage, hormone receptor status, and whether or not they want chemotherapy. After those treatment methods are decided, then patients will be randomized to either whole breast irradiation or partial breast irradiation.
What is the difference between Whole Breast and Partial Breast Irradiation?
For whole breast radaition patients will undeergo conventional treatment methods and dosing schemes. As of now, the standard of care for radiation to the entire breast is to treat to a dose of 1.8Gy * 28 treatments for a total dose of 50.4Gy or to treat at 2Gy a day * 25 treatments for a total dose of 50Gy over 5 weeks. The fields must include all of the breast tissue, and NO regional nodes. Patients may receive an optional “boost” of radiation to the lumpectomy cavity with electrons to take the patient to a total dose of 66.4Gy as a maximum.

As you can see i nthe above picture, the cavity within the breast where the tumor was located needs to be defined well by the physician. According to the study, the cavity needs to be treated by 90% of the total perscription dose. This means that this area needs to receive at least 45.4Gy if you are treating to a total dose of 50.4Gy. In order to make sure that this cavity is included properly, surgeons would either leave clips behind when they removed the tumor, and then physicians would make sure to give a 2cm margin around this area. The other technique would be for the patient to have a CT scan done, and when the plan is being created, that the lumpectomy site be contoured by the physician to ensure that the site + 2cm would be treated to at least 90% of the perscription dose.
A plan would look much like this picture then:
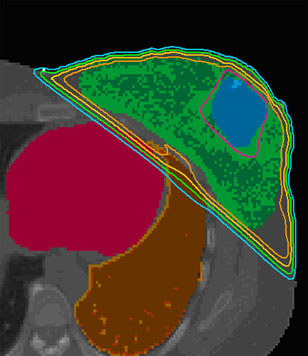
You can see that the blue volume represents where the tumor was located at the time of surgery. The pink line that surrounds it would represent the 90% of the total prescription dose that the physician wants to treat the entire breast to. The green painted area represents the entire breast tissue that is being treated with the prescription dose. The last thing that needs to be considered, is that the cavity itself has to be less then 35% of the total breast volume. Meaning women with small breasts that may have had a larger 3cm mass may not be eligible for the study.
For the partial breast irradiation portion of the study, women would either have high dose rate brachtherapy using catheters, the Mammosite option, or with external beam radiation. Ideally, patients would be given 2 treatments a day, with at least 6 hours in between each treatment, over 5 to 10 days, for a total of 10 treatments. The difference in the number of days would depend on the facility patients would be treated at, patient schedules, and ability to schedule 2 treatments a day.
For Mammosite, patients would be treated with 3.4Gy * 2 daily treatments * 5 days for a total of 34Gy. The balloon must also be able to be as close to a perfect circle as possible. There can NOT be more then a 2mm difference in the circumference of the balloon at any point in space. There needs to be at least 5mm between the edge of the Mammosite balloon and the skin surface. Ideal it would be greater then 7mm, but 5mm is the minimum. Here is where things gets a bit confusing. Physicians need to be able to limit the amount of radiation that the entire breast recieves with this technique, so less then 60% of the entire breast tissue can receive greater than or equal to 50% of the total prescription dose. Since we are treating such a small volume, it should not be a problem.
In this example you can see that the balloon is perfectly symetrical. The dose is covering the balloon appropriately and the there is far less then the study required 60% or less of the breast tissue receiving 50% of the total prescription dose. Mission accomplished. However, this patient was a bit tricky since the dose did get a bit close to the skin, and was about 5mm away from the skin surface versus the ideal 7mm or greater. What this does is increases the potential for a skin reaction with the treatment. It would not be anything terrible and cause a large skin burn, or for the skin to blister, but if it can be avoided, it is best for the patient.
The other technique that could be used is called Breast Brachytherapy with the use of multiple catheters. Here is an example of what that looks like:

The treatment parameters for this technique are identical to that of the Mammosite technique. The only difference is that this technique uses more catheters to surround the lumpectomy site, as well as go directly through it. The other difference is that instead of having the dose coverage go 2cm beyond the balloon like in Mammosite, it only has to go 1.5cm beyond the lumpectomy cavity. This is due to that fact that there are more catheters surrounding the cavity site, and allowing for a better dose coverage around the area. This is what a plan might look like with this technique:

Significance of this study?
According to the current standards of care, patients receive whole breast radiation to lessen the chances of have a recurrence else where in the breast. According to at least 5 randomized prospective trials that have compared the outcomes of patients treated with WBI versus lumpectomy alone. In these trials there has been no difference in the number of patients have a recurrnce in the opposite unaffected breast, or in other areas of the same affected breast. Where the benefit has been seen is in the lumpectomy cavity itself. If a patient is going to recur, it is highly likely for that patient to recur at the site of the original tumor site in the breast, provided that it is a Stage 0, 1, or 2 breast cancer. So these studies have shown in fact that Radiation Therapy offers a benefit to the local control at the site of the orginal tumor, but that it has no clincally significant benefit to the rest of the breast tissue.
Previous studies have also shown that less then 10% of patients will have little cancerous lesions greater then 1cm away from the original tumor site. Due to this fact alone, these patients are good candidates for this trial as well. There was also a study done by the physicians at Ochsner Clinic involving patients with DCIS and the use of interstitial brachytherapy (multicatheter system). This study concluded that there was a substantially low percentage of patients that recurred after their treatments. Meaning that mulit catheter brachy therapy to the breast for DCIS was highly effective in controling the chance for local recurrence.
In the 20 year update of the study by Veronesi et al examining the equivalence of standard BCT to mastectomy, the incidence of new cancers developing in the same breast but in different areas of the breast were exactly the same as those patients chances for having a breast cancer in the opposite breast. This suggests that elective treatment with RT beyond the tumor bed itself provides minimal benefit to patients. There are similar findings by the Yale group as well. In a 15-year update on 1152 patients treated with conventional WBI, the Yale Group found that there was only a 13% chance for women to develop a new cancer in a different location in the breast from where the original site tumor was located.
Can an acceptable outcome be achieved with RT delivered only to the region of the tumor bed?
If this were the case, radiation therapy could be delivered in 1 to 2 weeks, thus significantly shortening treatment time and potentially reducing health care costs. A shortened treatment schedule would decrease the burden of care for patients undergoing Breast Cancer Therapy, thus making available the conservation option for more women. By reducing the length of time required to deliver RT, the logistical problems associated with integrating local and systemic therapies would also be eliminated. Additionally, toxicity to adjacent normal structures (i.e., heart, underlying chest wall, contralateral breast) should be reduced significantly by decreasing the volume of irradiated tissue.
This is the main prupose for this entire study. I hope this helps to shed some more light on this Phase III Trial.
As always, if you or a loved one have any other questions, comments, or concerns; if you would like more information in regards to another cancer related topic, please contact me at: CANCERGEEK@GMAIL.COM or CANCERGEEK@CANCERGEEK.COM
~CancerGeek


Sue
Posted at 05:55h, 10 OctoberDetecting breast cancer early is when it is easiest to treat. It may mean life or death, or it may mean mild treatments versus more toxic treatments.